01
Virtual Nursing
RemoteICU’s Virtual Nurses provide 24/7 clinical support that relieves your team
Learn more
Solving Physician Shortages with
Advanced Telemedicine Solutions
and Remote Clinicians
Improving Patient Care For Hundreds of Hospitals, Since 2008
RemoteICU is a leading provider of remote specialist physician services. We improve patient care by enabling enhanced clinician provision and performance, while helping address chronic and ever-increasing shortages in specialist physician coverage for hospitals of all sizes. Our physicians collaborate with your local personnel and follow your clinical protocols. Since our establishment, RemoteICU has proudly grown into one of the world’s largest telemedicine groups comprised of licensed specialist physicians, with our footprint extending across six continents.

RemoteICU’s Impact In Numbers
Of Patient Beds
Of Hospitals
Continents

01
RemoteICU’s Virtual Nurses provide 24/7 clinical support that relieves your team
Learn more

03
We provide hospitals with Tele-ICU shifts (eICU), for existing and new Virtual ICUs
Learn more
04
Our Internal Medicine telehospitalists cover the smallest to the largest hospitals
Learn more
05
Our teleneurologists perform general neurology, in addition to tPA administration for stroke via TeleStroke
Learn more
06
Our telemedicine coverage is replicated and performed for all inpatient or outpatient specialties
Learn more
Improve clinical outcomes while decreasing the costs of care per patient
Our easily accessible advanced technology allows your physicians to perform more effectively
Fill your specialist shortages and regular scheduling gaps with licensed physicians who desire a permanent position
The total cost of adding RemoteICU is comparable to hiring a new physician locally
With 24/7 accessibility, RemoteICU physicians maintain uninterrupted monitoring of patients to provide improved treatment
Our physician specialists will cover your hard to fill night, weekend and holiday shifts
Improved work conditions decrease the burden on your in-house team and increase staff satisfaction and retention
Staff your hospital unit with our qualified specialists to meet the Leapfrog Physician Staffing Standard
How we Work
You and our RemoteICU Medical Director will discuss your clinical needs in full detail.
RemoteICU will send a proposal to help address your coverage needs.
Your hospital can begin interviewing RemoteICU physicians without delay. RemoteICU will then credential physicians to permit them to become permanent members of your hospital staff.
RemoteICU’s IT specialists will coordinate with your hospital’s IT team and oversee all the arrangements.
Due to a rapid and simultaneous process, RemoteICU physicians will be able to perform their first shift within the soonest possible time frame.
A Small Hospital System's ICUs
A hospital system with two hospitals had only part-time in-house intensivist coverage. The critical care physicians would round on the ICU patients in the morning, but the physicians were not in the ICU most of the day. Patient issues which would arise in the ICUs after they had completed their rounds were often left to the hospitalists to manage. This was clearly suboptimal and did not meet accepted standards of ICU care. At night, ICU patients continued to be managed by hospitalists, who were also responsible for the management of non-ICU patients throughout the hospital. The intensivists were available from home by telephone, which meant that they had to be woken up if their expertise was needed. As such, they were only involved in the most urgent issues. Since they were at home, they had to rely on information relayed to them by the nurses or hospitalists as they did not have easy access to the EMR or the bedside telemetry. Management of less-acute problems were often postponed until the morning.RemoteICU was brought in to address these problems. RemoteICU enables a comprehensive ICU telemedicine solution, including technology and critical care board-certified physicians who are members of the hospital staff. The RemoteICU doctors are available from their workstations continuously, with instant access to the EMR, radiology images, and bedside telemetry as well as high-definition cameras in each room which enable them to assess the patients and to interact with them and/or their family members.
A Large Hospital System's ICUs
A large rural hospital had a “revolving door” of moonlighters and locum tenens doctors. This frequent staff turnover had a negative impact on the care being rendered in the ICU. The hospitalists and the bedside nurses found it quite challenging to always be working with and acclimating to new physicians.This often led to frustrating communications between nurses and doctors, discontinuity of patient care, and inconsistent adherence to hospital protocols. This arrangement was also quite costly to the hospital.RemoteICU was contracted to empower a comprehensive telemedicine technology solution, including a lineup of intensivists presented to the hospital clinical leadership for proposed acceptance to join their clinical staff, with no capital investment in infrastructure. This new intensivist stability has improved the quality and the consistency of the ICU care and has improved ICU staff satisfaction. This also enabled the hospital to attain Leapfrog compliance, a high priority for this hospital.
Large Hospital Neurology
A large hospital had too few neurologists on staff to handle their large number of acute stroke cases. Therefore, the hospital had outsourced their stroke coverage to a tele-stroke provider, but they were often dissatisfied with the timeliness of the neurologists’ responses. The hospital turned to RemoteICU to provide neurologists who would join their permanent physician staff and would be dedicated to covering only their hospital and its related facilities. RemoteICU coordinated a no capital investment comprehensive telemedicine solution, including staff neurologists who not only cover tele-stroke cases but who also would perform tele-neurology consults. This has satisfied the hospital’s tele-stroke and tele-neurology needs.
Large Hospital System Hospitalist
A large hospital system had bedside hospitalists who were too busy with the large volume of admissions and calls they were expected to handle.The hospital turned to RemoteICU to provide additional hospitalists to enhance coverage of the hospital and its associated inpatient facilities thereby correcting the hospital’s clinical personnel shortage. The tele-hospitalists work hand-in-hand with the bedside hospitalists and nurses. Patient and clinical staff are now much more satisfied since their needs are being met in a more-timely manner.
A Large Hospital With One Individual Hospital in Need of ICU Coverage
A single hospital with a small intensive care unit (7 beds) was compelled to transfer out many of their acute patients because they did not have a physician who was qualified to manage complicated acute cases, including mechanically ventilated patients. As a result, most of the patients requiring ICU level of care were being transferred to a distant hospital to receive ICU care. RemoteICU was brought in to manage these critically ill patients. This has enabled the hospital to keep the vast majority of these patients thereby improving the continuity of care and retaining more of the revenues that these patients generate.
What’s On People’s Mind
October 12, 2023
In recent years, the healthcare industry has witnessed a remarkable evolution, with technology playing a pivotal role in reshaping the way patient care is delivered. The concept of eICU, short for electronic Intensive Care Unit, has emerged as a game-changer, offering new possibilities for providing critical care. This digital innovation has made headlines and continues to shape the healthcare landscape as it addresses contemporary challenges, such as the recent COVID-19 pandemic, by enhancing patient care and improving resource allocation.
eICU is a telemedicine system that connects off-site critical care specialists with patients in remote or understaffed hospitals, enabling real-time monitoring and intervention. This technology has gained significant attention during the pandemic, as it allowed experts to remotely monitor and consult on patients’ conditions, reducing the strain on overwhelmed healthcare facilities. By leveraging eICU, healthcare providers could efficiently allocate their resources and expertise, thereby improving patient outcomes.
This technology doesn’t only benefit critical care units; it also caters to rural and underserved communities. As healthcare disparities have been brought to the forefront during the pandemic, eICU has emerged as a solution to bridge the gap. By enabling remote consultations and expert guidance, eICU facilitates access to high-quality care for patients who might not have otherwise received it.
eICU also incorporates cutting-edge artificial intelligence (AI) and data analytics, further enhancing its capabilities. By processing vast amounts of patient data, it can predict deteriorating conditions and suggest interventions in advance, ultimately saving lives and resources. The intersection of AI and telemedicine has the potential to revolutionize patient care, particularly in critical situations.
In conclusion, eICU is not just a buzzword; it is the future of critical care in healthcare. With its real-time monitoring, remote expertise, and AI-driven insights, it has proven its mettle in the face of the COVID-19 pandemic and continues to redefine the way we deliver healthcare. As the world grapples with ongoing health challenges, eICU stands as a testament to the power of technology in improving patient outcomes and ensuring equitable access to quality care. Its relevance in current events cannot be overstated, and its influence is only expected to grow in the years to come.
(This blog entry was aided by non-human intel.)
October 3, 2023
In an era marked by rapid advancements in technology and the growing demand for efficient healthcare solutions, the term “eICU” has gained prominence in the medical landscape. This innovative approach to healthcare has the potential to reshape patient monitoring, improve outcomes, and alleviate the strain on healthcare systems, which has become increasingly critical in light of recent global events.
The acronym “eICU” stands for “electronic Intensive Care Unit,” a concept that has evolved with the integration of cutting-edge technology into healthcare. It involves a remote monitoring system that connects critical care specialists with patients in intensive care units (ICUs) through the use of telemedicine, data analytics, and real-time communication tools. This approach enables healthcare providers to extend their reach beyond the confines of a physical ICU, making it possible to monitor patients from a centralized hub regardless of geographical location.
Current events, particularly the global COVID-19 pandemic, have underscored the need for innovative healthcare solutions like eICU. The pandemic placed immense pressure on healthcare systems worldwide, leading to overcrowded ICUs and stretched medical resources. eICU emerged as a beacon of hope, offering a means to monitor and care for a greater number of patients with fewer physical staff present in the ICU. This technology allowed critical care specialists to remotely assess patient data, adjust treatment plans, and provide timely interventions, all while minimizing the risk of exposure to the virus.
Furthermore, eICU is not limited to pandemic responses; it is also a valuable tool for addressing the ongoing challenges of healthcare accessibility and resource allocation. In regions with limited access to specialized medical care, eICU can bridge the gap by connecting patients with expert healthcare professionals. This democratization of healthcare has the potential to enhance patient outcomes, particularly for those in underserved areas.
In conclusion, eICU represents a groundbreaking approach to healthcare monitoring that holds immense promise for the future. Its relevance and importance have been highlighted by recent global events, emphasizing the urgent need for innovative solutions to address the challenges facing healthcare systems. As eICU continues to evolve and gain traction, it has the potential to revolutionize patient care, improve outcomes, and make healthcare more accessible to all, regardless of geographic location or medical resources.
(This blog entry was aided by non-human intel.)
September 5, 2023
In today’s fast-paced world, where the demand for healthcare services is ever-increasing, the need for advanced and efficient medical care is more critical than ever. Recent advancements in technology have not only made our lives more convenient but have also revolutionized the way healthcare is delivered. One such groundbreaking innovation is the eICU system, which has been gaining momentum and proving its worth in enhancing physician performance.
In the wake of the COVID-19 pandemic, healthcare systems worldwide have faced unprecedented challenges. The strain on medical resources and personnel has been immense, highlighting the importance of technology-driven solutions like eICU. The eICU, or Electronic Intensive Care Unit, is a telemedicine platform that connects remote critical care specialists with bedside clinicians to monitor and manage patients in real-time. This remote monitoring system has not only improved patient outcomes but has also significantly elevated physician performance.
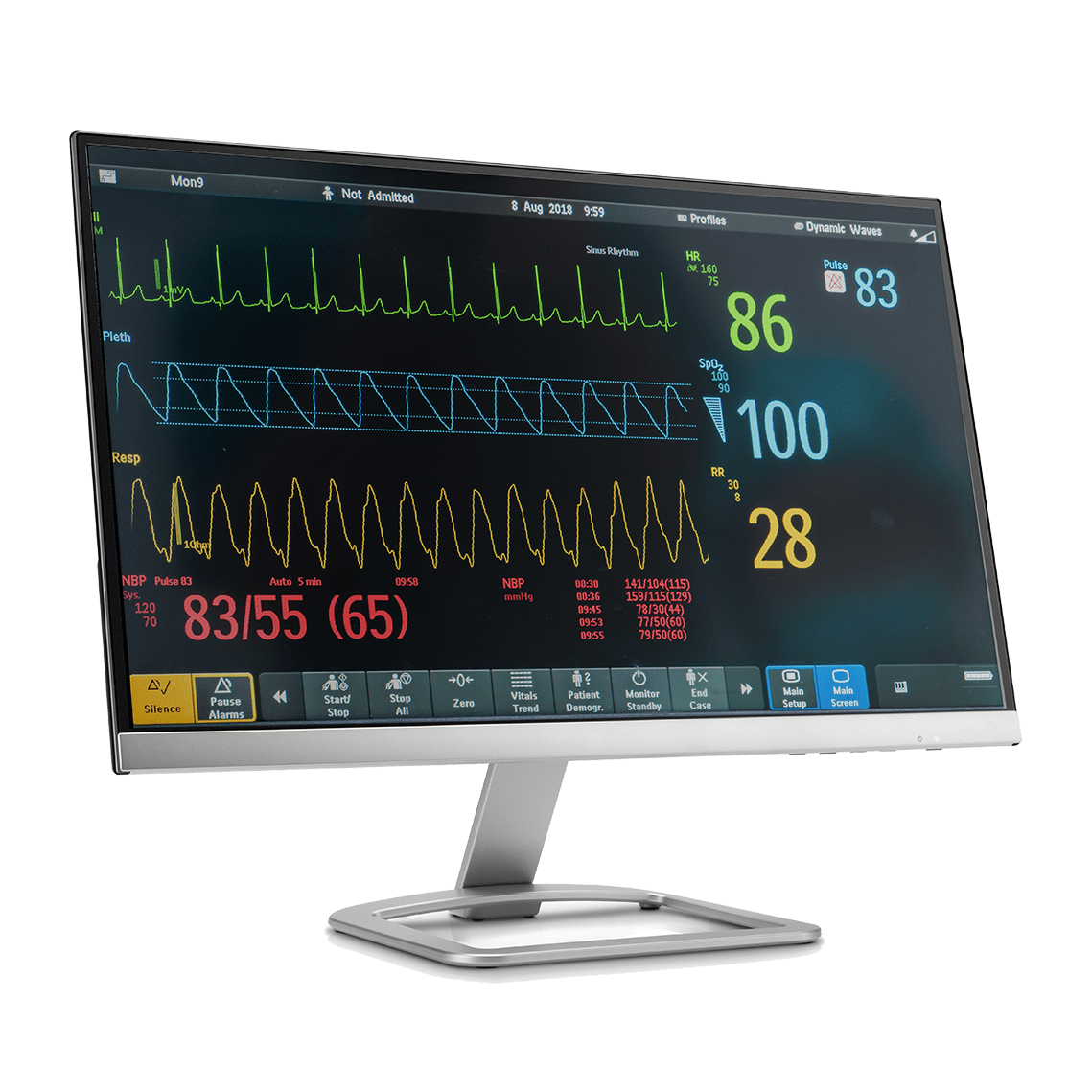
One of the key ways eICU technology enhances physician performance is by providing continuous access to critical patient data. Through a network of cameras, sensors, and electronic health records, eICU enables remote specialists to monitor patients’ vital signs, lab results, and treatment plans. This constant stream of information empowers physicians to make informed decisions promptly, reducing the risk of medical errors and improving patient care.
Additionally, eICU promotes collaboration among healthcare professionals. With the ability to consult with remote specialists, bedside clinicians can access expertise that might not be available in their local facility. This collaborative approach to patient care not only expands the knowledge base of physicians but also enhances their decision-making skills.
Furthermore, eICU technology has proven to be invaluable in addressing physician burnout, a prevalent issue in the healthcare industry. By reducing the burden of constant in-person monitoring, physicians can achieve a better work-life balance, leading to improved mental and emotional well-being. This, in turn, translates into more focused and effective patient care.
In conclusion, the eICU system has emerged as a transformative tool in the healthcare landscape, particularly in the context of current events like the COVID-19 pandemic. By providing continuous access to patient data, promoting collaboration among healthcare professionals, and mitigating physician burnout, eICU technology is undeniably improving physician performance. As we continue to navigate the complexities of modern healthcare, embracing innovations like eICU will be instrumental in achieving better patient outcomes and a healthier society.
(This blog entry was aided by non-human intel.)
August 28, 2023
In the fast-paced world of healthcare, technology continues to play an instrumental role in transforming patient care. One innovation that has gained significant attention is the concept of TeleICU, short for Tele-Intensive Care Unit. This groundbreaking approach combines the expertise of critical care specialists with the power of remote monitoring, ushering in a new era of patient management. In the backdrop of recent global events, the benefits of TeleICU have come to the forefront, demonstrating how it is not just a novel idea, but a necessary one.
TeleICU brings a unique blend of advanced technology and medical care to the table. The concept involves remotely monitoring and managing patients in intensive care units through real-time audio and video connections, coupled with cutting-edge data analysis tools. This approach bridges the geographical gap between patients and specialized critical care teams, ensuring that even the most remote medical facilities can access top-notch care.
The ongoing global health challenges have underscored the importance of TeleICU more than ever before. With the strain on healthcare systems, including shortages of critical care specialists and hospital beds, TeleICU emerges as a solution that provides expert guidance regardless of physical location. This capability has proven particularly valuable in ensuring equitable access to high-quality care, irrespective of a hospital’s geographical location or the larger medical crisis at hand.
TeleICU brings forth several distinct advantages. Firstly, it facilitates quicker response times, as remote specialists can intervene promptly, reducing the risk of complications. Secondly, it allows for continuous monitoring, with data-driven alerts that help avert potential crises. Thirdly, the knowledge sharing between on-site and remote teams ensures a holistic approach to patient care. Lastly, TeleICU aids in early patient rehabilitation by enabling tailored interventions, leading to swifter recoveries.
In the ever-evolving landscape of healthcare, TeleICU stands as a testament to the harmonious union of medicine and technology. As global events continue to reshape our world, the adoption of TeleICU highlights how innovation can enhance patient care delivery. From underserved regions to overwhelmed hospitals, the benefits of TeleICU reverberate across the medical spectrum. As we stride into the future, one thing is certain: the evolution of TeleICU is not just a trend, but an imperative step towards revolutionizing critical care on a global scale.
(This blog entry was aided by non-human intel.)
August 7, 2023
In the rapidly evolving landscape of healthcare, the integration of technology has led to revolutionary changes in patient care. One groundbreaking development that has garnered significant attention is the implementation of teleICU, a telemedicine solution that connects intensive care units (ICUs) with remote critical care specialists through advanced electronic monitoring systems. The convergence of technology and medical expertise in the eICU domain has opened up new avenues for improving patient outcomes, especially during times of crisis.
Managing the intricate logistics of a teleICU network is a multidimensional challenge that requires meticulous planning, seamless coordination, and cutting-edge technology. As the world faced the unprecedented challenges posed by the recent global health crisis, the significance of teleICU solutions became even more pronounced. Hospitals across the world found themselves grappling with the surge in critical patients, limited resources, and the need to ensure the safety of both patients and healthcare professionals.
TeleICU emerged as a vital tool to address these challenges. The ability to remotely monitor and manage critically ill patients allowed healthcare providers to efficiently allocate resources, provide timely interventions, and maintain a high level of care even when physical distancing measures were in place. In this context, the strategic deployment of teleICU became a central pillar of effective crisis management.
However, managing teleICU logistics is no simple feat. It involves a delicate balance of technology infrastructure, skilled personnel, and standardized protocols. Hospitals must invest in state-of-the-art monitoring equipment, ensure robust data security measures, and provide specialized training for teleICU staff. Furthermore, establishing clear communication channels between onsite ICU teams and remote specialists is essential for seamless information exchange and decision-making.
The success of teleICU implementation is a testament to the collaborative spirit of modern healthcare. It underscores the remarkable ability of the medical community to adapt and innovate in response to unforeseen challenges. As we reflect on recent events, it is evident that the integration of teleICU into healthcare ecosystems has not only elevated patient care during critical moments but has also set the stage for a more resilient and technologically empowered future.
In conclusion, navigating the complexities of teleICU logistics requires a comprehensive approach that encompasses technological prowess, skilled workforce, and effective communication. The recent global health crisis has demonstrated that teleICU is not just a concept but a tangible solution that has the potential to transform patient care. By embracing the challenges and opportunities presented by teleICU, healthcare providers can forge a path toward enhanced patient outcomes and a more robust healthcare system.
(This blog entry was aided by non-human intel.)
August 1, 2023
In recent years, the healthcare industry has witnessed remarkable technological innovations that have revolutionized patient care on a global scale. Among these advancements, teleICU (also known as eICU or tele-ICU) stands out as a game-changing approach to critical care.
TeleICU is a remote monitoring system that connects intensive care specialists to critically ill patients in distant locations through high-tech communication platforms. Regardless of geographical boundaries, teleICU provides expert critical care support to hospitals and healthcare facilities, ensuring timely interventions and improving patient outcomes. This technology enables access to a pool of skilled ICU professionals, bridging the gap between healthcare disparities in remote and underserved regions.
TeleICU has emerged as a vital tool in addressing healthcare disparities across the globe. In many developing countries, remote areas often lack access to specialized medical care, leading to higher mortality rates and reduced patient outcomes. TeleICU systems offer a lifeline to these regions, providing remote guidance to healthcare teams, enhancing diagnosis accuracy, and empowering local healthcare professionals to make well-informed decisions in critical situations.
The outbreak of global pandemics, such as the recent COVID-19 crisis, highlighted the importance of teleICU in managing large-scale emergencies. Overburdened healthcare systems faced unprecedented challenges, and teleICU played a significant role in optimizing resources and providing expert guidance remotely. The ability to monitor and support critical patients from a distance reduced exposure risks for medical staff, ensuring continuity in patient care during times of crisis.
TeleICU systems are backed by cutting-edge technologies, including artificial intelligence and data analytics. These tools enable real-time data monitoring, predictive analysis, and early warning systems, which aid in identifying deteriorating patients promptly. By leveraging data-driven insights, healthcare professionals can make informed decisions, reduce hospital stays, and decrease the overall cost of critical care.
The global perspective of teleICU demonstrates its potential as a transformative force in healthcare. By transcending borders, teleICU offers life-saving solutions to regions facing healthcare challenges and contributes significantly to improving patient outcomes worldwide. This advanced critical care approach, combined with the resilience showcased during recent global health crises, has cemented teleICU as a pivotal element in the future of medicine. Embracing teleICU technology not only empowers healthcare providers but also creates a more equitable healthcare landscape, where expertise knows no boundaries and patient care is enhanced through the power of connectivity and innovation.
(This blog entry was aided by non-human intel.)
July 19, 2023
In the dynamic realm of modern healthcare, advancements in technology have brought transformative changes to critical care management. TeleICU and traditional ICU are two prominent approaches that have gained significant attention. This article explores the key differences between these systems and their relevance to current events in the context of healthcare challenges and advancements.
TeleICU, a concept that emerged in the late 20th century, has garnered widespread adoption in recent years due to the growing demand for critical care services. Utilizing high-definition video conferencing, electronic health record integration, and real-time data analytics, teleICU enables remote monitoring and expert support to patients, regardless of geographical barriers. This remote monitoring capability offers several advantages over traditional ICU setups. It facilitates quicker response times, reduces the risk of adverse events, and provides access to specialized care, regardless of location. Additionally, teleICU optimizes resource allocation by efficiently distributing expert care across multiple sites, thus easing the burden on local healthcare facilities.
While teleICU presents promising opportunities, it also comes with its own set of challenges. Ensuring data security, protecting patient privacy, and integrating complex technology into existing healthcare systems require careful consideration. Additionally, maintaining the human aspect of patient care is crucial, as teleICU should complement, not replace, in-person care. Striking the right balance between technology and human touch is essential to providing comprehensive critical care.
The ongoing global health challenges, such as the COVID-19 pandemic, have highlighted the significance of teleICU in addressing surges in critical patients. In times of crisis, teleICU systems have played a crucial role in connecting overwhelmed hospitals with remote intensivists, easing the strain on frontline healthcare workers, and improving patient outcomes. The ability to remotely monitor and manage critical patients has proven invaluable during emergencies, demonstrating the potential of teleICU to adapt to current events and provide efficient and timely critical care solutions.
As we embrace the advancements in telemedicine, the teleICU model stands as a testament to the potential of technology in enhancing critical care services. By acknowledging its benefits, addressing challenges, and incorporating ethical considerations, teleICU can continue to play a vital role in shaping the future of critical care delivery. The ongoing global health challenges underscore the significance of teleICU in responding to emergencies and adapting to current events while ensuring optimal patient outcomes. As technology continues to evolve, teleICU will likely play an increasingly prominent role in advancing critical care in modern healthcare.
(This blog entry was aided by non-human intel.)
July 10, 2023
In today’s fast-paced world, technological advancements continue to reshape various industries, including healthcare. One such innovation making significant strides is teleneurology, a field that combines neurology and telemedicine to provide remote care for patients with neurological conditions. Amidst the ongoing healthcare challenges, teleneurology has emerged as a transformative solution, bridging the gap between patients and specialists, and reducing patient mortality rates. This article explores the profound impact of teleneurology on patient outcomes and its relevance in current events.
One of the critical aspects of teleneurology is its ability to facilitate telestroke consultations. Telestroke allows healthcare professionals to remotely assess and diagnose stroke patients in real-time, regardless of their geographical location. This approach has revolutionized emergency stroke care, enabling prompt treatment initiation, which is crucial for positive outcomes. The rapid response provided by telestroke consultations has proven to be a lifesaver, especially in regions with limited access to neurologists.
Teleneurology plays a vital role in reducing healthcare disparities by ensuring that patients, regardless of their location or socioeconomic status, can receive expert neurological care. In remote areas or underserved communities, access to neurological specialists may be limited, leading to delayed diagnoses and treatment. With teleneurology, patients can now connect with neurologists through video consultations, improving their chances of receiving timely interventions, reducing mortality rates, and enhancing overall quality of life.
The COVID-19 pandemic further highlighted the significance of telemedicine, including teleneurology, in delivering safe and efficient healthcare. Social distancing measures and overwhelmed healthcare systems necessitated remote patient care solutions. Neurologists quickly adapted to telehealth platforms, enabling ongoing management and monitoring of patients’ neurological conditions. Teleneurology emerged as a critical tool in safeguarding both patients and healthcare providers, ensuring continuous care and mitigating the risks associated with in-person visits during the pandemic.
Teleneurology has already demonstrated its potential to improve patient outcomes and reduce mortality rates. As technology continues to evolve, further advancements in remote neurological care can be expected. With the integration of artificial intelligence, remote monitoring devices, and data analytics, teleneurology has the potential to enhance diagnostic accuracy, optimize treatment plans, and provide personalized care. Moreover, ongoing research and development in this field will continually refine teleneurology’s capabilities, making it an indispensable component of modern healthcare.
Teleneurology’s ability to reduce patient mortality rates and improve outcomes is undeniable. This transformative approach to remote neurological care offers hope for patients in need, irrespective of their location or circumstances. By embracing teleneurology and leveraging its potential, healthcare providers and policymakers can contribute to a future where access to expert neurological care is not limited by physical boundaries. Teleneurology is not just a trend but a valuable tool driving positive change in current events and paving the way for a more inclusive and effective healthcare system.
(This blog entry was aided by non-human intel.)
July 5, 2023
In the era of digital transformation, healthcare has witnessed remarkable advancements, particularly in the realm of telemedicine. One revolutionary aspect of telemedicine is the electronic Intensive Care Unit (eICU), an innovative approach that integrates technology and critical care to remotely monitor and treat patients in intensive care units (ICUs). Amidst the ongoing global healthcare challenges, eICU has emerged as a beacon of hope, effectively reducing patient mortality rates.
By leveraging cutting-edge technology, eICU allows healthcare professionals to remotely monitor patients in real time, providing continuous surveillance of vital signs, laboratory results, and other critical data. This continuous monitoring enables early identification of deteriorating conditions, empowering healthcare teams to intervene promptly. In the context of recent events, the COVID-19 pandemic highlighted the crucial need for remote monitoring capabilities to effectively manage ICU patients while minimizing exposure risks for healthcare workers.
Another compelling aspect of eICU is its ability to facilitate seamless collaboration among healthcare teams. Through secure video conferencing and instant messaging, critical care experts can provide real-time guidance and support to on-site staff, regardless of geographical barriers. This virtual collaboration optimizes decision-making processes and ensures patients receive the best possible care. The current shortage of critical care specialists in various regions has further emphasized the importance of eICU in extending expert support to underserved areas.
eICU’s integration of advanced analytics and machine learning algorithms allows for early identification of clinical deterioration patterns. By analyzing vast amounts of patient data, eICU can generate predictive models that assist in detecting high-risk patients who may require immediate intervention. These data-driven insights can significantly reduce mortality rates by enabling proactive interventions and individualized treatment plans. With the rise of big data and artificial intelligence, eICU has the potential to revolutionize critical care on a global scale.
In an era where patient outcomes are paramount, eICU stands as a remarkable solution in reducing patient mortality rates. Its ability to provide enhanced surveillance, facilitate collaboration, and harness the power of predictive analytics holds immense potential. By staying at the forefront of technological advancements, healthcare organizations can leverage eICU to transform critical care delivery and ultimately save more lives. As the world embraces the digital revolution, eICU emerges as a testament to the power of technology in shaping the future of healthcare.
(This blog entry was aided by non-human intel.)
June 28, 2023
In today’s ever-evolving healthcare landscape, technological advancements continue to shape the way we approach patient care. One such innovation making waves is TeleICU, an exciting development in critical care medicine. Combining the power of telecommunication and intensive care, TeleICU brings specialized expertise to patients in remote locations, improving access, and potentially saving lives. This article explores the concept of TeleICU, its benefits, and its relevance in the context of current events.
TeleICU, also known as eICU or e-ICU, is a cutting-edge approach that connects off-site intensivist physicians and critical care specialists with patients in ICUs through advanced audiovisual technology. This remote monitoring system enables real-time patient assessments, consultation, and intervention, even when the medical professionals are physically located miles away. The COVID-19 pandemic has further highlighted the significance of TeleICU, as hospitals faced overwhelming patient volumes and strained healthcare resources.
With TeleICU, healthcare providers can remotely monitor patients, analyze vital signs, and provide timely interventions. By utilizing data analytics and predictive algorithms, TeleICU systems can detect subtle changes in patient conditions, allowing for early intervention and preventing adverse events. This technology offers a cost-effective solution, reducing the need for physical transfers, minimizing strain on healthcare staff, and optimizing resource allocation.
Furthermore, TeleICU has demonstrated its value in underserved rural areas and regions with limited access to specialized critical care expertise. By leveraging TeleICU systems, hospitals can ensure that patients receive high-quality care, irrespective of their geographical location. This inclusivity and equitable distribution of critical care services align with the current global healthcare focus on addressing disparities and improving healthcare access for all.
n conclusion, TeleICU represents a significant advancement in critical care, enhancing patient outcomes, and expanding access to specialized expertise. This technology-driven approach aligns with the ongoing pursuit of improving healthcare systems worldwide.
(This blog entry was aided by non-human intel.)
June 14, 2023
In the rapidly advancing landscape of healthcare technology, teleICU (also known as eICU or e-ICU) has emerged as a game-changing solution, revolutionizing critical care delivery. With the ability to remotely monitor and treat patients in intensive care units (ICUs), teleICU represents an affordable breakthrough that holds tremendous potential for improving patient outcomes. In this article, we will explore the cost-effective advantages of teleICU and discuss how recent developments have further solidified its position as a transformative force in healthcare.
TeleICU offers a cost-effective solution to traditional ICU care by leveraging technology to connect patients in remote locations with a centralized team of intensivists and critical care nurses. This virtual approach eliminates the need for physical presence, thereby reducing staffing costs, optimizing resource utilization, and streamlining workflow efficiency. The financial benefits of teleICU are particularly significant for rural hospitals or regions with limited access to critical care specialists, as it allows them to utilize the expertise of remote professionals without incurring high travel expenses or relocation costs.
There have been several notable developments showcasing the increasing adoption and positive impact of teleICU systems. A groundbreaking study published in a prominent medical journal demonstrated how teleICU reduced mortality rates by 26% among critically ill patients in a community hospital. The study’s findings underscored the potential of teleICU to bridge the gap between access and quality of care, providing life-saving interventions even in resource-constrained environments.
Furthermore, health systems and providers across the globe have recognized the immense value of teleICU solutions in managing the strain on healthcare infrastructure during the ongoing pandemic. With surges in COVID-19 cases, the implementation of teleICU programs has enabled hospitals to expand their critical care capacity efficiently, ensuring that patients receive timely and specialized care remotely.
TeleICU represents a cost-effective and accessible solution that democratizes critical care, bringing specialized expertise to patients who would otherwise face limited options. By optimizing resources, enhancing patient outcomes, and enabling healthcare providers to effectively navigate surges in demand, teleICU is poised to transform the landscape of critical care delivery. As the world embraces the potential of this groundbreaking technology, we can look forward to a future where quality critical care is available to all, regardless of geographical barriers or financial constraints.
(This blog entry was aided by non-human intel.)
June 12, 2023
Telemedicine has emerged as a game-changer in the healthcare industry, revolutionizing the way medical services are delivered. Among its many branches, tele-hospitalist medicine has gained significant momentum. This article explores the fascinating realm of tele-hospitalist medicine, shedding light on its role in advancing remote patient care. Additionally, we will examine recent events from the last week that highlight the growing significance of this field in modern healthcare.
Tele-hospitalist medicine refers to the practice of providing hospitalist care remotely through telecommunication technologies. In an era where access to medical expertise is critical, tele-hospitalist medicine plays a pivotal role in delivering comprehensive patient care beyond the physical boundaries of a hospital. This innovative approach allows hospitalists to remotely assess and monitor patients, collaborate with other healthcare professionals, and make informed decisions in real-time. By leveraging digital platforms, tele-hospitalist medicine ensures continuous care and optimal resource utilization.
In recent news, a renowned healthcare system successfully implemented a comprehensive tele-hospitalist program. This initiative aimed to address the challenges posed by the COVID-19 pandemic, ensuring uninterrupted care for hospitalized patients while minimizing the risk of exposure. By leveraging telemedicine technology, the program allowed hospitalists to remotely assess patients, provide consultations, and coordinate care with the onsite healthcare team. This recent event exemplifies how tele-hospitalist medicine is adapting to the current healthcare landscape, reinforcing its relevance in ensuring quality patient care amidst challenging circumstances.
Tele-hospitalist medicine brings numerous benefits to patients, including increased accessibility, timely interventions, and improved continuity of care. By leveraging telecommunication tools, patients can receive specialized care regardless of their geographical location, reducing the need for unnecessary transfers and associated inconveniences. Moreover, tele-hospitalist medicine fosters collaboration among healthcare professionals, ensuring comprehensive and coordinated care delivery.
As the healthcare industry continues to embrace digital advancements, tele-hospitalist medicine stands at the forefront, offering innovative solutions to enhance remote patient care. Recent events, such as the successful implementation of tele-hospitalist programs, highlight the growing importance of this field in providing seamless, patient-centered care. By leveraging telemedicine technologies, tele-hospitalist medicine holds the potential to revolutionize healthcare delivery, ensuring optimal outcomes and improved access to medical expertise in the digital age.
(This blog entry was aided by non-human intel.)
June 8, 2023
In the ever-evolving landscape of healthcare, advancements in technology continue to revolutionize patient care and access to specialized services. One such area that has gained significant attention in recent years is tele-neurology, a branch of telemedicine focused on providing neurological care remotely. Within this field, telestroke has emerged as a groundbreaking approach to revolutionize the way stroke patients receive critical care. In this blog post, we explore the current state of tele-neurology and telestroke, while highlighting recent developments that underscore their importance in modern healthcare.
Tele-neurology is a subfield of telemedicine that utilizes telecommunications technology to provide neurological consultations and care to patients who are geographically distant from specialists. It enables neurologists to assess, diagnose, and treat patients with neurological conditions remotely, utilizing videoconferencing and other digital platforms. Telestroke, a key component of tele-neurology, specifically focuses on delivering time-sensitive stroke care, including the administration of thrombolytic therapy, to patients in remote or underserved areas.
Research studies published in leading medicals journal have demonstrated the efficacy of telestroke consultations in significantly reducing the time to treatment for stroke patients. The study, conducted across multiple hospitals, found that patients who received telestroke consultations had a significantly higher likelihood of receiving thrombolytic therapy within the recommended time frame compared to those who received in-person consultations only.
The studies’ findings reinforce the growing body of evidence supporting the effectiveness of telestroke as a means to improve stroke care accessibility and outcomes. They also highlight the potential for tele-neurology to bridge the gap between underserved communities and specialized neurological expertise, addressing disparities in healthcare access.
Tele-neurology and telestroke represent game-changing innovations in the field of stroke care, bringing specialized expertise directly to the patient’s bedside, regardless of their physical location. As the recent study underscores, these technologies have the potential to revolutionize stroke care by expediting critical interventions and improving patient outcomes. Embracing these advancements and investing in tele-neurology infrastructure will help ensure that all stroke patients, regardless of their geographic location, receive timely and effective care, thus making significant strides in reducing the devastating impact of strokes on individuals and communities worldwide.
(This blog entry was aided by non-human intel.)
June 6, 2023
In today’s rapidly advancing digital landscape, the field of healthcare is embracing innovative technologies to improve patient care and revolutionize medical practices. One such groundbreaking development is the implementation of teleICU, an advanced telemedicine system that connects critically ill patients in remote locations with intensive care specialists. With the rise of eICU or electronic ICU, this cutting-edge solution is reshaping the way diagnoses are made, fostering timely interventions, and ultimately saving lives.
The world has witnessed the remarkable utilization of teleICU systems in response to the emergence of a new and highly contagious respiratory illness. In regions heavily affected by this outbreak, hospitals have implemented eICU programs to bolster their diagnostic capabilities and provide real-time critical care support. This integration of telemedicine into ICU settings has not only facilitated quicker diagnoses but has also allowed medical experts to remotely monitor and manage patients’ conditions, even when physical contact is limited.
Enhancing Diagnoses through TeleICU: TeleICU empowers healthcare providers with an unparalleled ability to make accurate diagnoses promptly. By leveraging high-definition video conferencing, patient data sharing, and real-time vital sign monitoring, specialists can remotely assess patients’ symptoms, examine medical imaging, and collaborate with on-site healthcare teams to develop tailored treatment plans. Furthermore, these digital platforms enable specialists to access comprehensive patient histories, laboratory results, and medication records, providing a holistic perspective to aid in accurate diagnoses.
Remote Expertise and Timely Interventions: The integration of teleICU into healthcare systems bridges geographical barriers, granting patients in underserved areas access to a network of highly skilled intensive care professionals. This remote expertise ensures that even in regions lacking specialized resources, patients can receive timely diagnoses and appropriate interventions. Moreover, teleICU systems allow for continuous monitoring of critical patients, notifying specialists of any alarming changes in vital signs or clinical parameters. This rapid response capability can significantly improve patient outcomes by facilitating early interventions and preventing complications.
Conclusion: As technology continues to evolve, teleICU stands at the forefront of transforming critical care and diagnosis processes. The recent surge in its implementation, driven by the need for remote healthcare during global events, underscores its efficacy in overcoming geographical limitations and delivering expert diagnoses. By embracing teleICU, healthcare systems can harness the power of real-time connectivity, enabling accurate diagnoses, facilitating timely interventions, and ultimately improving patient outcomes in the digital era.
(This blog entry was aided by non-human intel.)
May 31, 2023
In today’s dynamic healthcare landscape, technology continues to reshape the way we deliver care, improving patient outcomes and bridging gaps in staffing challenges. TeleICU, also known as eICU or e-ICU, has emerged as a revolutionary solution that utilizes remote monitoring and communication technology to address the difficulties of filling weekend, night, holiday, and other hard-to-fill shifts. In this article, we will explore the significance of teleICU and its transformative impact on healthcare.
TeleICU offers a cutting-edge approach to critical care by connecting remote critical care specialists with on-site teams through advanced technology. By leveraging real-time monitoring, high-definition cameras, and secure communication systems, teleICU enables experts to virtually support and collaborate with clinicians in intensive care units (ICUs). This innovative solution has the potential to revolutionize healthcare delivery, ensuring optimal care is available round the clock.
One of the most significant benefits of teleICU is its ability to address staffing challenges during challenging shifts. Weekends, nights, holidays, and other hard-to-fill shifts often face shortages, which can impact patient care. With teleICU, healthcare organizations can tap into a network of critical care specialists who provide virtual support, ensuring continuous monitoring, expert guidance, and timely interventions. This bridge between supply and demand helps alleviate strain on local staff and enhances patient safety.
TeleICU’s remote monitoring capabilities empower critical care specialists to proactively identify potential complications, intervene promptly, and optimize treatment plans, resulting in improved patient outcomes. Through constant surveillance of vital signs, remote experts can detect subtle changes, mitigate risks, and make timely interventions. This real-time collaboration between on-site and remote clinicians ensures that patients receive the highest quality of care, regardless of the time of day.
By leveraging teleICU technology, healthcare organizations can enhance efficiency and staff satisfaction. Remote specialists not only fill shift gaps but also alleviate the burden on on-site teams. This support reduces burnout, improves staff morale, and enhances job satisfaction. Moreover, the collaboration between local and remote experts fosters a culture of continuous learning and knowledge exchange, which ultimately benefits patient care.
TeleICU represents a transformative solution that addresses staffing challenges, enhances patient care, and optimizes critical shifts in healthcare. Through remote monitoring and collaboration, teleICU enables continuous support, expert guidance, and timely interventions during weekends, nights, holidays, and other challenging shifts. As healthcare continues to evolve, the adoption of teleICU promises to revolutionize critical care delivery and usher in a new era of improved patient outcomes and staff satisfaction.
(This blog entry was aided by non-human intel.)
May 25, 2023
In the wake of the COVID-19 pandemic, advancements in healthcare technologies have played a vital role in revolutionizing patient care. One such innovation that has gained significant attention is the eICU, also known as the electronic Intensive Care Unit. This article explores how eICU has transformed critical care and its relevance in the context of recent events.
The Impact of COVID-19: We are witnessing the global healthcare system continue its battle against the remaining impact of the pandemic. The lasting effects of COVID-19 have highlighted the urgent need for advanced and scalable healthcare solutions. As hospitals faced overwhelming patient loads, the importance of remote monitoring and efficient resource allocation became increasingly evident.
eICU: Reinventing Critical Care: eICU is an innovative telemedicine approach that leverages technology to enhance critical care delivery. With a network of remote monitoring stations, skilled intensivists and critical care nurses can remotely monitor patients in multiple ICUs simultaneously, irrespective of geographical barriers. This real-time monitoring system allows healthcare professionals to constantly evaluate patient data, including vital signs, lab results, and radiology reports, enabling early intervention and prompt decision-making.
The Role of Artificial Intelligence: Artificial intelligence (AI) has emerged as a key component of the eICU system. By analyzing vast amounts of patient data, AI algorithms can identify patterns, detect anomalies, and provide predictive insights. This technology assists healthcare providers in diagnosing and managing critical conditions, optimizing treatment plans, and reducing medical errors. Recent advancements in AI algorithms have further enhanced the accuracy and efficiency of eICU systems.
Addressing Post-Pandemic Challenges: As the world grapples with the aftermath of the pandemic, eICU technology has become even more crucial. It allows healthcare systems to expand their critical care capacity, effectively managing patient surges and preventing overwhelming scenarios. Moreover, eICU enables hospitals to provide specialized care to patients in remote or underserved areas, bridging the gap in access to critical care facilities.
Conclusion: eICU has emerged as a game-changer in the healthcare industry, transforming critical care delivery in a post-pandemic world. By leveraging advanced technologies like telemedicine and AI, eICU systems enable remote monitoring, early intervention, and efficient resource allocation. As we navigate the lasting effects of COVID-19, embracing such transformative solutions will be instrumental in ensuring resilient healthcare systems that can adapt to future challenges.
(This blog entry was aided by non-human intel.)
May 23, 2023
In today’s rapidly evolving healthcare landscape, technological advancements have played a pivotal role in revolutionizing the delivery of medical care. One such innovation is the implementation of TeleICU, alternatively referred to as eICU or e-ICU. This cutting-edge solution combines the power of telecommunication and intensive care expertise to remotely monitor patients in critical care units, enhancing physician performance and ultimately improving patient outcomes. This article delves into the potential of TeleICU in optimizing physician performance and its relevance in modern healthcare.
The Role of TeleICU in Healthcare Advancements:
Healthcare systems are currently grappling with the need for efficient resource utilization, particularly in intensive care units. Ageing populations, an upsurge in chronic conditions, and a shortage of critical care specialists have intensified the demand for innovative solutions. In response, healthcare institutions have turned to TeleICU as a means to bridge the gap and maximize physician efficiency.
Enhancing Physician Performance:
Amplified Reach: TeleICU empowers physicians to remotely monitor and oversee patients in multiple critical care units simultaneously. By utilizing video conferencing, real-time data analysis, and predictive algorithms, physicians can extend their expertise beyond physical boundaries, providing invaluable guidance to on-site medical teams.
Continuous Surveillance: With TeleICU, physicians can remotely monitor patients round the clock, ensuring constant surveillance of vital signs, lab results, and medical trends. Instant access to real-time data enables physicians to promptly identify deteriorating conditions, allowing for timely interventions and potentially preventing adverse events.
Collaborative Consultations: TeleICU facilitates seamless collaboration among healthcare professionals, promoting a multidisciplinary approach to patient care. Physicians can consult with specialists, share expertise, and collectively make informed decisions, fostering optimal treatment plans and reducing medical errors.
Augmented Decision-Making: TeleICU systems harness advanced analytics and artificial intelligence to process vast amounts of patient data, unveiling trends, risk factors, and treatment options. This augmented decision-making support assists physicians in accurate diagnoses, tailored treatment plans, and predictions of patient outcomes.
In the quest for efficiency and optimal resource utilization in healthcare, TeleICU emerges as a transformative technology. By leveraging the power of remote monitoring, real-time data analysis, and enhanced collaboration, physicians can elevate their performance and deliver high-quality care to a larger patient population. Embracing the potential of TeleICU empowers healthcare professionals to meet the challenges of an ever-evolving medical landscape, ultimately leading to improved patient outcomes and a brighter future for critical care medicine.
(This blog entry was aided by non-human intel.)
May 15, 2023
TeleICU, the use of telemedicine in intensive care units, is revolutionizing critical care delivery and addressing the challenges associated with locum tenens physicians. By leveraging technology to remotely monitor and manage intensive care patients, teleICU offers a compelling alternative to traditional locums. This article explores how teleICU serves as an effective solution to staffing shortages and ensures uninterrupted care for critically ill patients.
TeleICU serves as an alternative to locum tenens physicians, effectively addressing the challenges posed by staffing shortages. Traditionally, locums have been relied upon to fill temporary gaps in critical care staffing. However, their availability can be limited, leading to compromised patient care and increased workload for existing medical teams. TeleICU overcomes these challenges by connecting critically ill patients with remote intensivists who can provide continuous monitoring, timely interventions, and specialized expertise. This ensures that patients receive uninterrupted care, regardless of staffing constraints.
Through teleICU, remote intensivists have the ability to access real-time patient data, such as vital signs, lab results, and imaging, enabling them to make informed decisions and provide specialized care. The use of advanced technology, including video conferencing and secure data transmission, facilitates seamless communication and collaboration between the remote intensivists and the on-site medical teams. This collaborative approach ensures that critical care patients receive the highest level of expertise and attention, even in the absence of locum tenens physicians.
Furthermore, teleICU helps alleviate the burden on existing medical teams by redistributing the workload. By connecting with remote intensivists, the on-site medical staff can collaborate, seek guidance, and benefit from the expertise of specialists without the need for physical presence. This not only improves patient care but also enhances the well-being and job satisfaction of the medical professionals.
In conclusion, teleICU represents a transformative solution to the challenges associated with locum tenens physicians and staffing shortages in critical care units. By connecting critically ill patients with remote intensivists, teleICU ensures uninterrupted care, access to specialized expertise, and collaborative decision-making. As teleICU continues to evolve and become more prevalent, it has the potential to redefine critical care delivery and improve patient outcomes, ultimately revolutionizing the field of intensive care medicine.
(This blog entry was aided by non-human intel.)
May 11, 2023
In recent years, the healthcare industry has been revolutionized by the emergence of teleICU, an innovative approach to remote patient monitoring that utilizes advanced technology to connect critically ill patients in remote locations with healthcare professionals in real-time. The eICU, also known as the electronic intensive care unit, is a form of teleICU that allows for remote monitoring of critically ill patients by intensivists and critical care nurses through the use of advanced technology, such as videoconferencing, electronic health records, and remote monitoring devices.
As healthcare professionals face increasing pressure to manage an overwhelming number of patients, teleICU has emerged as a promising solution for reducing physician burnout. Recent studies have shown that teleICU can not only improve patient outcomes, but also provide valuable support for healthcare professionals, particularly those working in high-stress environments such as intensive care units.
Recent events have highlighted the importance of teleICU in reducing physician burnout. In the wake of the COVID-19 pandemic, healthcare professionals have been pushed to the brink as they struggle to keep up with the influx of patients requiring critical care. TeleICU has provided a lifeline for healthcare professionals, allowing them to remotely monitor and manage patients from a safe distance, reducing the risk of exposure to the virus while still providing high-quality care.
Beyond the pandemic, teleICU has the potential to transform the healthcare industry as a whole, reducing physician burnout and improving patient outcomes. As healthcare organizations continue to adopt teleICU technology, it is critical that they provide the necessary training and resources to ensure that healthcare professionals are able to effectively utilize these tools to improve patient care and reduce burnout.
In conclusion, teleICU represents a transformative approach to remote patient monitoring that has the potential to significantly reduce physician burnout and improve patient outcomes. As the healthcare industry continues to evolve, teleICU will undoubtedly play a key role in shaping the future of critical care.
(This blog entry was aided by non-human intel.)
May 4, 2023
Providing quality healthcare in rural areas has been a challenge for many years. The shortage of critical care specialists in these areas has made it difficult to provide the necessary care for critically ill patients. However, in recent years, teleICU has emerged as a promising solution to this problem. TeleICU refers to the use of telemedicine technologies to provide intensive care services remotely to critically ill patients in remote or underserved areas. It has been shown to improve patient outcomes, reduce healthcare costs, and improve the efficiency of healthcare delivery.
TeleICU is a vital tool that enables critical care specialists to provide care remotely using advanced telemedicine technologies such as high-definition video, secure messaging, and real-time data monitoring. It also enables critical care specialists to provide consultations to local healthcare providers, helping them make informed decisions about patient care.
The benefits of teleICU are numerous, especially in rural areas. TeleICU allows for early identification of critical illnesses, which can improve patient outcomes and reduce the length of hospital stays. It also enables healthcare providers to monitor patients remotely, reducing the need for transfer to urban hospitals, which can be costly and stressful for patients and their families. Additionally, teleICU can help reduce healthcare costs by reducing the need for expensive medical transport and unnecessary hospitalizations.
In conclusion, teleICU has the potential to revolutionize healthcare delivery in rural areas. It is a vital tool that can help address the shortage of critical care specialists in these areas, improve patient outcomes, and reduce healthcare costs. As healthcare continues to evolve, teleICU will likely play an increasingly important role in providing quality care to patients in remote and underserved areas.
(This blog entry was aided by non-human intel.)
May 2, 2023
In recent years, the healthcare industry has been at the forefront of adopting cutting-edge technologies to enhance patient care, and one such technology that has been gaining attention is TeleICU. TeleICU, also known as eICU, is an innovative technology that utilizes telecommunication and artificial intelligence to provide remote critical care to patients.
TeleICU is a game-changer for healthcare professionals who work in critical care, as it allows them to monitor and communicate with patients in real-time, regardless of their location. This technology connects the bedside team to a remote team of critical care specialists, who can monitor patient data and intervene when necessary.
One of the key benefits of TeleICU is its ability to reduce the workload of healthcare professionals and improve patient outcomes. The technology allows for round-the-clock monitoring, which ensures that any changes in a patient’s condition are immediately identified and addressed.
TeleICU is also cost-effective, as it eliminates the need for on-site critical care teams. This makes it an attractive option for hospitals that have limited resources and struggle to attract and retain critical care specialists.
Furthermore, the use of artificial intelligence in TeleICU has the potential to revolutionize critical care even further. AI can analyze large amounts of patient data and identify patterns that may indicate potential complications before they occur. This allows for proactive intervention, which can save lives and reduce the need for invasive procedures.
In conclusion, TeleICU powered by AI is a beneficial innovation that has the potential to transform the way we deliver critical care. With its ability to provide remote monitoring, reduce the workload of healthcare professionals, and improve patient outcomes, it is clear that TeleICU is a game-changer for the healthcare industry. As hospitals continue to face challenges in providing quality care to patients, TeleICU is proving to be an invaluable tool in delivering critical care, regardless of the location of the patient.
(This blog entry was aided by non-human intel.)
April 27, 2023
TeleICU technology, also known as eICU or e-ICU, has revolutionized critical care by enabling remote monitoring and management of critically ill patients using real-time data analysis and videoconferencing. While the technology has been widely adopted in the United States, its impact has been felt globally, particularly in areas with limited critical care resources.
In recent news, teleICU technology has been highlighted for its potential to address critical care shortages in countries like India and Brazil. In India, teleICU technology has been implemented in multiple states to address critical care shortages in rural areas. In one instance, a teleICU program in the state of Punjab provided remote critical care support to patients in rural areas.
Similarly, in Brazil, teleICU technology has played a critical role in managing critically ill patients, particularly in areas where critical care resources are limited. In one instance, a teleICU program in Sao Paulo provided remote critical care support to hospitals in the northern state of Amazonas, which was overwhelmed by a surge in critically ill patients.
Beyond critical care shortages, teleICU technology has also been used to address critical care disparities in remote and rural areas. In India, for instance, teleICU technology has been implemented to provide remote critical care support to patients in rural areas where access to critical care expertise is limited. The technology has also been used to provide critical care support in disaster-stricken areas, such as during the 2018 Kerala floods, where a teleICU program provided remote critical care support to flood victims.
Despite its potential, teleICU technology still faces challenges in the global context, particularly in areas with limited internet connectivity and resources. However, as the technology continues to evolve and become more affordable, it has the potential to transform critical care globally, improving patient outcomes and reducing mortality rates in areas with limited critical care resources.
In conclusion, teleICU technology has the potential to advance critical care globally, particularly in areas affected by critical care shortages and disparities. As the technology continues to evolve and become more accessible, it has the potential to improve patient outcomes and save lives in areas where critical care expertise is scarce.
(This blog entry was aided by non-human intel.)
April 23, 2023
As technology continues to advance in the medical industry, teleICU, or electronic ICU, has become a promising solution to improve patient care and outcomes. TeleICU is a remote monitoring system that connects intensivists and critical care nurses to patients in the ICU via audiovisual technology, allowing for 24/7 monitoring and management.
Recent events have highlighted the importance of teleICU, with the ongoing COVID-19 pandemic overwhelming hospitals and leading to a shortage of ICU beds and staff. TeleICU has allowed hospitals to expand their critical care capacity and provide remote support to frontline healthcare workers.
According to a report by Market Research Future, the global teleICU market is expected to grow at a CAGR of 16.5% from 2021 to 2028, driven by factors such as the increasing prevalence of chronic diseases, rising demand for remote patient monitoring, and technological advancements.
One of the key benefits of teleICU is the ability to provide real-time monitoring and intervention. This can lead to improved patient outcomes, such as reduced mortality rates and shorter ICU stays.
Another benefit of teleICU is the potential cost savings. By providing remote monitoring and support, hospitals can reduce the need for on-site staffing and equipment, leading to lower operating costs. A study by the University of Massachusetts Medical School found that teleICU implementation resulted in a 30% reduction in ICU costs.
However, there are still challenges to the widespread adoption of teleICU. One major challenge is the cost of implementation and maintenance of the technology. Additionally, there are concerns about patient privacy and data security.
Despite these challenges, the future looks promising for teleICU. As the technology continues to improve and become more affordable, it has the potential to revolutionize critical care and improve patient outcomes on a global scale. With the ongoing pandemic and the increasing demand for remote healthcare solutions, teleICU is poised to play a vital role in the future of healthcare.
(This blog entry was aided by non-human intel.)
April 20, 2023
With the healthcare industry constantly evolving, technological advancements are at the forefront of the progress. One such advancement is the eICU, or electronic intensive care unit, which is also referred to as TeleICU. TeleICU is a system that enables healthcare providers to remotely monitor critically ill patients in intensive care units (ICUs) using advanced monitoring technologies.
In recent years, TeleICU has gained significant attention in the healthcare industry due to its many benefits. The system allows doctors and nurses to remotely monitor patients in real-time, providing critical information needed to make informed decisions. Additionally, TeleICU can help address the shortage of critical care specialists in rural and remote areas by providing access to highly specialized care from a distance.
One significant benefit of TeleICU is improved patient outcomes. The system has been shown to reduce the length of stay in the ICU, decrease the risk of complications, and improve survival rates. The remote monitoring also provides support to bedside healthcare providers, ensuring that patients receive timely interventions.
In the last week, there have been discussions surrounding the future of TeleICU and its potential to revolutionize the healthcare industry. As the world continues to face challenges in healthcare delivery, TeleICU has the potential to address some of the most significant challenges, including accessibility, efficiency, and cost-effectiveness.
In conclusion, TeleICU is a significant technological advancement that has the potential to improve patient outcomes and revolutionize the healthcare industry. As the technology continues to advance, the future of TeleICU looks promising. With the ability to remotely monitor patients in real-time, TeleICU provides healthcare providers with the critical information needed to make informed decisions, ultimately improving patient care. The system has the potential to address some of the most significant challenges in healthcare delivery, making it an essential tool for the future.
(This blog entry was aided by non-human intel.)
April 18, 2023
In recent years, the field of critical care has witnessed a remarkable transformation with the advent of eICU or e-ICU technology. As healthcare continues to evolve, eICU has emerged as a cutting-edge approach to patient monitoring and care delivery, leveraging the power of technology to revolutionize critical care units.
Recent events have highlighted the increasing need for innovative solutions in critical care, making eICU a timely topic of discussion. With hospitals grappling with challenges such as limited resources, staffing shortages, and rising patient volumes, eICU has gained renewed attention as a potential game-changer in the field.
So, what exactly is eICU? At its core, eICU is a telehealth concept that involves remote monitoring and virtual care for critically ill patients. Using state-of-the-art technology, data analytics, and real-time monitoring, eICU allows for continuous oversight and management of patients in intensive care units (ICUs), regardless of their physical location.
The benefits of eICU are manifold. By leveraging remote monitoring, eICU enables healthcare providers to closely monitor multiple patients simultaneously, facilitating early detection of potential complications and prompt intervention. This not only helps improve patient outcomes but also enhances the efficiency of critical care units, optimizing resource utilization and reducing the burden on frontline healthcare workers.
Moreover, eICU has also been shown to reduce the length of ICU stays and lower mortality rates, making it a promising tool in critical care management. The ability to remotely access and analyze patient data in real-time empowers healthcare providers with valuable insights for making informed decisions, even from a distance.
In conclusion, eICU has emerged as a groundbreaking approach to critical care, leveraging the power of technology to enhance patient monitoring and care delivery. With its potential to optimize resource utilization, improve patient outcomes, and address the challenges faced by critical care units, eICU is undoubtedly shaping the future of critical care. As healthcare continues to evolve, the integration of eICU technology is poised to revolutionize critical care and pave the way for more efficient and effective patient care.
(This blog entry was aided by non-human intel.)
April 13, 2023
In today’s rapidly evolving healthcare landscape, eICU (also known as e-ICU) is emerging as a game-changer in critical care. By leveraging the power of telemedicine and data analytics, eICU is transforming how patients in intensive care units (ICUs) are monitored and managed, leading to improved outcomes and enhanced patient care.
In recent news, the role of eICU has gained prominence in managing critical care during natural disasters and emergencies. With the increasing frequency and severity of natural disasters, such as hurricanes, wildfires, and floods, healthcare facilities can be overwhelmed with patients requiring critical care. eICU provides a solution by enabling remote monitoring and management of patients in affected areas, ensuring timely interventions and optimized resource utilization during such crises.
One of the key strengths of eICU is its ability to collect and analyze vast amounts of patient data in real-time. Advanced sensors, monitors, and electronic health records (EHRs) capture and transmit data to a central command center, where critical care teams can remotely monitor patients’ vital signs, lab results, and other clinical parameters. Data analytics and AI algorithms then process this information, providing insights and actionable alerts to healthcare providers, enabling proactive care interventions and reducing the risk of adverse events.
eICU also bridges the gap between expertise and geographical limitations. In underserved or remote areas, where access to specialized critical care may be limited, eICU allows patients to receive remote monitoring and management from experienced critical care clinicians. This facilitates timely interventions and ensures that patients receive the same quality of care regardless of their location, reducing disparities in healthcare delivery.
In addition to improved patient outcomes, eICU has shown potential cost savings. By reducing complications, hospital length of stay, and unnecessary transfers, eICU can lower healthcare costs, making it a cost-effective solution for hospitals and healthcare systems.
In conclusion, eICU is changing the landscape of critical care by leveraging telemedicine and data analytics to remotely monitor and manage critically ill patients. With its ability to provide real-time monitoring, access to expertise, and potential cost savings, eICU has the potential to enhance patient care and optimize resource utilization, especially during natural disasters and emergencies. As technology continues to advance, eICU is poised to play an increasingly significant role in critical care management, unlocking new possibilities and improving patient outcomes.
(This blog entry was aided by non-human intel.)
April 9, 2023
The ongoing COVID-19 pandemic has brought unprecedented challenges to healthcare systems worldwide, particularly in the management of critical care patients. As hospitals grapple with surges in patient volumes and overwhelmed frontline healthcare providers, telemedicine solutions such as eICU and e-ICU have emerged as innovative tools that are shaping the future of critical care.
In recent news, the utilization of eICU and e-ICU has been on the rise as hospitals strive to provide optimal care to critically ill COVID-19 patients. With the ability to remotely monitor and manage ICU patients, these telemedicine platforms have played a crucial role in mitigating the strain on healthcare systems during the pandemic.
In hotspot areas with overwhelmed hospitals and limited access to critical care specialists, eICU and e-ICU have enabled remote monitoring and management of patients, facilitating early detection of deteriorating conditions, and timely interventions. This has proven to be particularly valuable in regions with high COVID-19 patient volumes, where the demand for critical care services has surged, and resources have been stretched thin.
Furthermore, eICU and e-ICU have been effective in minimizing exposure risks for frontline healthcare providers. By allowing remote monitoring and management of patients, these telemedicine platforms have reduced the need for direct contact, thus mitigating the risk of transmission and protecting healthcare workers from potential exposure to the virus.
The cost-effective benefits of eICU and e-ICU have also been noteworthy. By optimizing resource utilization, reducing ICU length of stay, and preventing complications, these telemedicine solutions have helped hospitals improve efficiencies and manage limited resources during the pandemic.
However, challenges related to patient privacy, data security, and technological infrastructure remain. As the utilization of eICU and e-ICU continues to expand, it is crucial to ensure robust protocols and regulations are in place to address these concerns effectively.
In conclusion, eICU and e-ICU have emerged as pioneering solutions in the age of COVID-19, reshaping the landscape of critical care. These telemedicine platforms have provided remote monitoring and management of ICU patients, addressing the challenges posed by the pandemic and offering unprecedented opportunities to improve patient outcomes, protect frontline healthcare providers, and optimize resource utilization. As the world continues to navigate the evolving healthcare landscape, eICU and e-ICU stand as crucial tools that are shaping the future of critical care and redefining the way healthcare is delivered in the face of unprecedented challenges.
(This blog entry was aided by non-human intel.)
April 6, 2023
While implementing a Tele-ICU program does not necessarily have upfront costs, hospitals can break even or even see cost savings over time through a number of mechanisms. Here are some ways that hospitals can break even or save costs with Tele-ICU:
Improved patient outcomes: Studies have shown that Tele-ICU programs can lead to improved patient outcomes, such as reduced mortality rates, reduced lengths of stay, and reduced rates of complications. These improved outcomes can lead to cost savings for the hospital.
Reduced staffing costs: Tele-ICU programs can allow hospitals to leverage the expertise of intensivists and other critical care specialists across multiple hospitals, potentially reducing the need for local staffing in some areas. This can lead to reduced staffing costs for the hospital.
Reduced transfers: Tele-ICU programs can help hospitals manage critically ill patients more effectively, potentially reducing the need for patient transfers to other facilities. This can lead to cost savings for the hospital and improve patient outcomes.
Increased efficiency: Tele-ICU programs can allow for more efficient use of hospital resources, such as ICU beds and equipment. This can lead to reduced costs and improved patient flow through the hospital.
Improved revenue: Tele-ICU programs can help hospitals attract and retain patients who may prefer the added layer of critical care support. This can help increase patient volume and revenue for the hospital.
Overall, while Tele-ICU programs do not necessarily have upfront costs, they have the potential to provide significant cost savings and other benefits over time. Hospitals should carefully evaluate the costs and benefits of Tele-ICU implementation and consider these potential mechanisms for cost savings and revenue generation.
(This blog entry was aided by non-human intel.)
April 5, 2023
In today’s world, technology is constantly evolving and transforming every sector. The healthcare industry has also experienced a significant shift with the integration of technology in patient care. One such technological advancement is the eICU or electronic ICU, which has revolutionized critical care in hospitals.
eICU refers to a system that uses advanced telecommunication technologies to monitor critically ill patients in intensive care units (ICUs) from remote locations. The eICU system is a collaborative effort between critical care doctors, nurses, and technology experts who work together to provide continuous care to critically ill patients. The system uses advanced sensors and monitors to collect patient data and transmit it to a centralized location where a team of critical care professionals monitors and analyzes the data. The team can then make timely interventions to improve patient outcomes.
The eICU system has several benefits. One significant advantage is that it allows remote access to critical care specialists, even in rural areas where such expertise may not be available. This improves patient outcomes as specialists can provide timely interventions and manage critical situations. Additionally, the system reduces the workload of ICU staff, allowing them to focus on direct patient care. The eICU system also uses data analytics to identify trends and patterns in patient data, enabling proactive interventions to prevent complications.
The eICU system has gained immense popularity in recent times. Many hospitals have implemented the system, and studies have shown a significant reduction in ICU mortality rates with its use. Furthermore, the eICU system has proven to be cost-effective in terms of reducing hospital stays, readmission rates, and overall healthcare costs.
In conclusion, the eICU system is a prime example of how technology can improve patient care in critical care settings. Its remote monitoring capabilities, data analytics, and timely interventions have transformed the way ICU care is delivered. The eICU system has shown remarkable results, improving patient outcomes and reducing healthcare costs. As technology continues to advance, we can expect further innovations in healthcare, and the eICU system is a shining example of how technology can make a positive impact on patient care.
(This blog entry was aided by non-human intel.)
April 2, 2023
The world is becoming increasingly digital, and healthcare is no exception. Telemedicine, the practice of delivering healthcare services remotely, has been around for a while, but it has recently gained traction due to the COVID-19 pandemic. Tele-neurology and telestroke are two types of telemedicine that are revolutionizing stroke care.
Tele-neurology is the use of telemedicine technology to diagnose and treat neurological conditions. Telestroke, on the other hand, is a subfield of tele-neurology that focuses specifically on stroke care. Telestroke allows healthcare providers to diagnose and treat strokes remotely, eliminating the need for patients to travel to a hospital or stroke center.
One of the main benefits of telestroke is speed. Stroke is a time-sensitive condition, and the faster it is diagnosed and treated, the better the patient’s outcome. Telestroke enables healthcare providers to diagnose and treat strokes faster than traditional methods. For example, a patient in a rural area who experiences a stroke can receive immediate care from a neurologist located in a city hospital.
Another benefit of telestroke is access to specialized care. Many hospitals do not have a stroke specialist on staff, so patients in these areas may not receive the best possible care. Telestroke allows patients to receive care from stroke specialists regardless of their location.
Telestroke also reduces healthcare costs. Stroke patients who receive treatment remotely are less likely to require hospitalization, which can be costly. Additionally, telestroke eliminates the need for patients to travel long distances to receive care, which can be expensive.
Despite its many benefits, telestroke still has some limitations. For example, it may not be appropriate for all patients, especially those with complex medical conditions. Additionally, telestroke requires a reliable internet connection and specialized equipment, which may not be available in all areas.
In conclusion, tele-neurology and telestroke are changing the way stroke care is delivered. These technologies allow patients to receive faster, more specialized care, while reducing healthcare costs. As technology continues to advance, it is likely that telestroke will become even more prevalent in stroke care.
(This blog entry was aided by non-human intel.)
March 29, 2023
The COVID-19 pandemic has pushed the boundaries of technology in healthcare, accelerating the adoption of telemedicine solutions. One of the most prominent examples is the virtual ICU or TeleICU, which is changing the way critical care is delivered to patients. TeleICU leverages remote monitoring and communication technologies to provide real-time support and decision-making for patients in intensive care units (ICUs). Among the most popular TeleICU solutions is the eICU program developed by Philips, which has been in operation for over two decades.
The eICU program is a cloud-based platform that connects ICUs in different locations to a central hub staffed by critical care specialists. The system collects patient data from medical devices, electronic health records, and bedside cameras, which is then analyzed using advanced algorithms and artificial intelligence. The critical care team can monitor patients remotely, make recommendations, and intervene when necessary, reducing the risk of adverse events and improving outcomes.
The benefits of eICU and TeleICU are numerous. First, they allow for a more efficient use of critical care resources, as fewer specialists are needed to cover multiple sites. This also reduces the workload and burnout of critical care providers. Second, eICU and TeleICU can improve patient outcomes by providing early intervention and reducing complications. Studies have shown that eICU can reduce ICU mortality by up to 30% and ICU length of stay by up to 20%. Third, TeleICU can enhance access to critical care for underserved communities, rural areas, and remote locations.
The future of TeleICU is bright, with ongoing developments in AI, machine learning, and robotics. For example, some companies are exploring the use of drones to transport medical supplies and medications to remote ICUs, while others are developing wearable devices to monitor patients outside the hospital. However, there are also challenges to overcome, such as privacy and security concerns, regulatory barriers, and the need for more specialized training for critical care providers.
In conclusion, eICU and TeleICU are revolutionizing critical care by leveraging the power of technology to provide remote monitoring, decision-making, and support to patients in ICUs. As the COVID-19 pandemic has shown, telemedicine is not only a convenient option but also a necessary tool in times of crisis. The future of TeleICU is promising, and we can expect to see more innovations and advancements in this field in the years to come.
(This blog entry was aided by non-human intel.)
March 26, 2023
In recent years, technology has transformed many aspects of healthcare, including critical care. Three terms that have emerged in this space are eICU, virtual ICU, and TeleICU. While these terms may seem interchangeable, they refer to slightly different concepts. eICU refers to a remote monitoring system that provides critical care to patients in the ICU from a remote location. Virtual ICU is a similar concept, but the care team is physically located in the same hospital as the patient. TeleICU is another remote monitoring system that is similar to eICU.
These technologies have several benefits that make them promising for the future of critical care. One of the primary advantages of eICU, virtual ICU, and TeleICU is that they can improve patient outcomes. With continuous monitoring, these systems can detect changes in a patient’s condition quickly and provide treatment recommendations that can help prevent complications. A study published in the Journal of Critical Care found that eICU was associated with a 26% reduction in mortality rates among ICU patients.
Another benefit of eICU, virtual ICU, and TeleICU is that they can increase efficiency in ICU resource utilization. These systems allow for remote monitoring of multiple patients by one team of specialists. This can reduce the burden on ICU staff and allow for better allocation of resources. It can also help prevent costly complications and readmissions, ultimately resulting in cost savings for healthcare facilities.
eICU, virtual ICU, and TeleICU can also help address staffing shortages, particularly in rural areas. These technologies allow remote teams of specialists to provide critical care, which can be especially beneficial in areas where there is a shortage of ICU specialists.
Additionally, these technologies can help improve communication between healthcare providers. The remote monitoring system allows for real-time data exchange between healthcare professionals, allowing for faster and more effective decision-making. It can also reduce the likelihood of errors or misunderstandings that can occur with traditional communication methods.
Despite the benefits, there are some challenges to implementing eICU, virtual ICU, and TeleICU. One concern is the cost of the technology and the training required for staff. Additionally, there may be resistance from some healthcare providers who prefer traditional methods of care delivery. However, as the healthcare industry continues to evolve, it is likely that these technologies will become more prevalent in critical care settings.
In conclusion, eICU, virtual ICU, and TeleICU are innovative technologies that have the potential to transform critical care. These remote monitoring systems offer a range of benefits, including improved patient outcomes, more efficient use of ICU resources, and cost savings for healthcare facilities. As the healthcare industry continues to embrace technology, it is likely that eICU, virtual ICU, and TeleICU will become more widely adopted, improving the quality of care for ICU patients.
(This blog entry was aided by non-human intel.)
February 7, 2023
This past week concluded Arab Health, an expansive annual conference hosted in Dubai, United Arab Emirates, which addresses all topics related to healthcare pertinent to the Arab world (i.e., all of healthcare). Having started close to 50 years ago actually, the conference sees major representations from all Persian Gulf states and beyond. This year was no exception with solid presence from the UAE of course, Saudi Arabia, Bahrain, and Qatar.
Of note, all Gulf states would benefit from telemedicine, without exception, and particularly from inpatient telehealth, and even more precisely, Tele-ICU. Let’s look at Dubai Healthcare City in the Emirates. Among other reasons, a primary driver for the creation of DHC is a venue for medical tourism, for those to travel into the UAE, to get high quality healthcare. And, in the case of Emirati nationals and residents, to avoid medical tourism, i.e., so they are less likely to see any benefit of traveling abroad to get specialized or otherwise high quality care (which of course goes hand in hand with the corollary, which is to highlight and obviate the negative of being far from home and family in the UAE which receiving care when traveling abroad for such purposes). It certainly makes sense for DHC to have the world’s most qualified experts treating their patients, whether the physicians are treating DHC patients remotely via telehealth or at the bedside. With regard to eICU, it’s much better even if you’re from Abu Dhabi, to have a family member treated by the world’s best physicians, in Dubai, rather than going let’s say to Germany for intensive care treatment, to speak nothing of the risks associated with transferring a patient, let alone the increased risks of a long distance transfer and especially over an international border, and even further since it would require multiple airports and a multi-hour flight.
Let’s look at the Kingdom of Saudi Arabia for a moment. A vast space, it’s similar to the United States in many key ways. Geographic distance is always an important factor in telemedicine and in particular with Tele-ICU. In other words, the more far flung critical patients are in more isolated and less populated areas, the less likely there are to be the most qualified specialist ICU physicians there. So, again, to get the best treated even within the Kingdom could means having to travel to a large city like Jeddah or Riyadh, and there are risks with traveling. Sometimes depending the acuity level of the patient, travel of any distance, even to a regional center, is simply is impossible.
RemoteICU is well positioned to organize TeleICUs in any Gulf state, having been involved in projects in the region for years, and can also provision permanent physician staff at the hospitals to monitor patients.
January 5, 2023
One can hardly open healthcare news and without finding an article relating to the terrible financial pressure facing hospitals in today’s environment. Not only do we have overall economic uncertainty, uncertainty with inflation and the job market, supply chain issues continuing to plague us (pardon the pun), but also many hospitals are seemingly on the brink of collapse. Telecritical care, eICU, and telehealth overall have the power to reduce costs in a major way. Those who are informed as to the powers of telemedicine to harness cost savings do themselves have the potential to do wonders for their careers as hospital administrators and executives and medical directors. Those who instead either sit on their hands or otherwise degrade the quality of care provided in the hospitals, providing less than what their patients deserve, indeed minimizing what they provide to their patients by decreasing the expertise utilized at their hospitals actually do so shortsightedly. It is done at their own peril and to the disadvantage of their patients. No patient in America today deserves less than the standard of care. Of course it saves money in the short run to terminate physicians and to have non-physicians treat patients instead. But is that really what patients deserve? It seems clear that that isn’t what patients deserve.
August 10, 2022
Naturally, predicting the future is valuable in any medical setting, and the ICU is of course no exception. Artificial intelligence is a means of The lack of availability (shortage of) intensivists is a central theme to many discussions relating to intensive care. The case for the eICU would not be as compelling without a dearth of board-certified critical care doctors. (It’s also important to note that a “board certified critical care doctor” is a physician who is board certified specifically in critical care by one of the boards capable of officially recognized certification in critical care, for example: the board of internal medicine, the board of surgery, etc. I.e., it would not be fair to say that a board certified internal medicine doctor who practices critical care in the ICU – which is very common – is generally what is meant by a “board certified critical care doctor” even though the IM doctor is indeed board certified and is also a physician who is a critical care doctor).
This shortage of boarded intensivists is exists in the context of — and is perpetuated by – an aging US population, coupled with an increase in the number of hospital ICU beds (and the proportion of ICU beds vs. total hospital beds). Further, increases in the prevalence of technology and the generally greater acceptance that there is value in a greater amount of data being captured/used, have created an environment where there is more data available to an ICU physician to enhance decision-making and judgement.
Companies and groups have endeavored to harness historical data for computer analysis in the creation of algorithms designed to predict the future. In other words, software was developed to examine whether complex statistical correlations exist between and among historical variables which then correspond to a certain clinical outcome or diagnosis some amount of time in the future. Sepsis would be one such outcome. Therefore when the same set of variables are captured in real time for a current patient and fed into a computer model, the algorithm would predict a diagnosis would occur in the future with some probability of accuracy, and before even the best doctor would be able to predict the same diagnosis.
It’s interesting how some terms and expression become dominant in typical parlance despite the intentions of academia or capital interests, and artificial intelligence (AI) as applicable the ICU is no exception. You may hear AI, machine learning (ML), decision support, decision tools, algorithmic assistance, RPM – remote proactive physiologic predictive monitoring, predictive tools, predictive monitoring, big data driven support, software-assisted clinical judgement, early warning systems, sepsis deterioration software, deterioration scoring system, robotic medicine, Sepsis Sniffer, and so on, being invoked. Regardless of the parlance, they are all essentially referring to artificial intelligence. A prime environment for such application is with eICU although it can also be equally useful in the bedside ICU.
Various groups and entities are pursuing standalone products or add-ons which aim to contribute in this realm, with various motivations, from performance to profit: Clew, Epic, Philips, Ceiba, and so on.
August 9, 2022
If you answered, “Accelerating adoption” you are correct. There are other correct answers of course, albeit obvious: “Telemedicine.” But one assumes the reader has that baseline knowledge already.
The ever-increasing burden on healthcare providers is due in part to a lack of adequate resources in non-urban areas and a simultaneous deficit of specialist physicians where they are needed. Non-urban areas for the purpose of this discussion also include remote areas and poorly developed, low economic strata areas. Simply put, there are not enough doctors.
Focusing on the United States for a moment, clearly the country is fully interconnected by telephone, so in theory a specialist physician is always only a phone call away. But that is theoretical only because the rural hospital in need has to have the capital resources to pay for a physician’s time and the physician’s telephone number must be known and the physician must be available and the physician has to be licensed in the state where the patient is located the have hospital privileges and credentials, all of which are non-trivial assumptions.
There is also a lack of immediacy in the chaos of a critical situation when clinical providers are frantically trying to find even a telephone number of someone to reach out to, meanwhile the clock is ticking. It’s said that in stroke situations, time is money, meaning every second counts toward saving the patient’s life. It’s no time to be searching for phone numbers. A potential stroke patient needs absolutely immediate assessment via videoconferenced tests done on the patient by a trained neurologist with stroke expertise. Additionally the neurologist must review neurological images in order to make rapid diagnoses, and to decide whether to administer alteplase by IV line, consideration of thrombolysis, and whether the patient needs to be “shipped out” (i.e.,) transferred for invasive procedures like thrombectomy, etc.
A telestroke neurologist can additionally interpret brain computed tomography and make decisions of whether to transfer for management of hemorrhagic stroke, to neurosurgical treatment facilities. Tele-stroke physicians use the National Institutes of Health Stroke Scale (NIHSS). This is merely scratching the surface of the activities and capabilities what tele-stroke physicians and how they work hand-in-glove with eICU intensivists and other remote specialist doctors and nurses.
While remote stroke care requires at least some technology to make it function, and its results are supported by studies analyzing its quality / metrics, other highly specialized tele-activities are much the same.
Telecardiologists have remote access to ECGs and ECHOs (eletrocardiograms and echocardiograms) and ideally should also have two-way video communication with the bedside staff and patient in the hospital bed. Clearly although there has been cardiac care advancement in recent decades, cardiovascular disease is still the #1 leading cause of death across the United States. It behooves hospital systems to have a tele-cardiology program in place.
August 7, 2022
Deadly diagnoses like sepsis are often well-suited for telemedicine, in part, especially with the adaptation of eICU. One of the major causes of mortality in hospitals is sepsis. Indeed billions of dollars are spent treating sepsis; it is one of the most cost-contributing conditions in a hospital and accounts for between and by some estimations accounts for between a third and a half of ICU dollars spent. To the extent that sepsis can be diagnosed sooner in a given case, statistically outcomes improve. For over 20 years a professional collaborative called the Surviving Sepsis Campaign put forth guidelines for sepsis treatment, but there is far less than full adoption of the protocols among hospitals across the United States and the developed world. Part of wider acceptance of the protocols would be greater availability of expert clinicians in intensive care medicine. Due to the shortage of intensivists and because of the poor economics of placing a costly intensivist in person at the bedside in a hospital where he or she would be working at less than full capacity utilization, it is compelling to use Tele-ICU to alleviate the poor sepsis protocol adaptation problem.
Of note, it’s not just intensive care units where there is lackluster adherence to sepsis protocols, but also emergency departments. Tele-intensive care physicians can also help out with septic patients in the ED, or in determination that they are in fact not septic, i.e., diagnosis via eICU’s remote monitoring and care provision capabilities when staffed by US board certified critical care doctors.
Also of note, algorithmic tools developed using artificial intelligence trained on physiologic data such as from MIMIC (or MIMIC-III an MIMIC-IV and so on), show promise in early sepsis detection. Various startups have tried to make inroads with software for this purpose, as well as larger electronic medical record companies.
August 4, 2022
If you accept a basic concept and reality of modern medicine which is that instead of like in the early 1900s there were predominantly general practitioner physicians who did basically everything for any given patient regardless of the patient’s ailment, as opposed to today where there are increasingly specialized and sub-specialized physicians such as surgeons and cardiologists and nephrologists and endocrinologists and neurologists and, yes, intensive care specialist physicians (intensivists), and that these specialized physicians pursue their specialties and obtain officially accepted board certification in those specialties and then they naturally produce better clinical outcomes for patients in their area of expertise then, no, you cannot simply have your ICU patients treated by nurses alone and expect clinical outcomes to be as favorable vs. if they were treated by specialist doctors. You cannot expect lengths of stay to be as short without doctors. You cannot expect mortality to be as low. You can expect more malpractice lawsuits, higher costs, and a poorer reputation for your hospital.
The intensive care unit is a less understood field at a basic level by laymen versus, say, surgery. Laymen understand that surgery must be performed by a surgeon who is of course a physician. Laymen would not accept major surgery being performed by a nurse. Many patients are brought to the ICU in an unconscious state and even if not they don’t choose their intensivist physician like they choose their dermatologist or surgeon, i.e., based on a recommendation or referral. In fact they typically don’t choose the physician at all and may not notice their physician is not a physician at all. During Covid and especially during the peaks and lockdowns, family isn’t allowed in the hospital, let alone in the ICU so there wouldn’t have even been an opportunity for either the patient — if the patient were conscious — or the family to take note that the ICU in question were not being managed by intensive care physicians but actually was being managed by internal medicine doctors who are hospitalists who are doing ICU work or nurses, but in either case neither hospitalists or nurses are board certified in critical care, which means that that scenario does not meet today’s standard of care, and clinical outcomes are expected to be worse or stated more directly more people are expected to die and lengths of stay are expected to be longer. Few people would find that situation acceptable. But just because laymen and their families do not notice you aren’t meeting the standard of care doesn’t mean your hospital will not pay the price of not having eICU coverage with malpractice claims, massively inflated operational costs of having patients stay longer in the ICU than would otherwise be, reputation costs, etc.
The Leapfrog group ranks hospitals by various criteria and when it comes to the hospital’s ICU, patients have to be managed by a US board certified critical care doctor. The ICU patient can be managed remotely by a TeleICU doctor or in person by a bedside ICU doctor, but either way, to be in conformity with the Leapfrog standard that physician has to be board certified in critical care, and of course that means that provider has to be a physician. Any other provider is not sufficient to meet the de facto standard from Leapfrog.
The eICU solves this problem. RemoteICU can provide coverage to your hospital exclusively with us board certified critical care doctors managing patients via eICU.
July 22, 2022
Various terms are frequently invoked in TeleICUs and virtual ICU discussions, particularly in the planning stage. Reactive vs. proactive, COR, hub, etc. The reactive vs. proactive decision is based on the basic philosophy of the eICU and is also tied to finance and budgets (and therefore rather than being strictly philosophical the decision can be determined just by the reality of finance and cost limitations), so naturally it gets a lot of attention. A proactive virtual ICU protocol means that the physicians or other clinicians (RNs, for example) working in the TeleICU act in advance to deal with expected difficulties or changes, in a sense trying to anticipate problems with patients by routinely checking certain things in their medical charts, telemetry, etc. It is a mindset and policy whereby the clinicians try to better the situation by trying to identify emerging or existing problems in advance of when they would otherwise become known, in effect by causing the clinicians’ own behavior to change, rather than waiting for an alert or call from someone else or indication from a computer or alarm or machine after the problem or change happens. Reactive TeleICU on the other hand is simply “putting out fires,” though of course not literally; you can imagine that firefighters would typically get a call to alert them that there is a fire on 131 Main Street and they “react” to the call by going to put out the fire. To continue the analogy, they are not ordinarily driving around proactively looking for fires that there is no indication or information exist. Some eICUs are so busy that the physicians are constantly only reacting to calls from the bedside whereby the remote intensivists in the hub (the offsite control center where the intensivists works at a computer to handle such calls in which the doctor has the EMR, PACS (radiology), ICU waveforms, etc., for the patient) responds with counsel and actions (orders) to be put on the patient. If the eICU physicians are so busy with reactive teleICU that they have no time remaining for proactive work, one way to increase the bed count coverage footprint of that virtual intensive care unit would be to add another simultaneous remote intensivist seat to work alongside the existing doctor which of course has cost implications.
July 21, 2022
The CDC indicated that 78% of the new infections in the last week were due to BA.5. This extraordinarily transmissible subvariant of the Greek letter-named variant “Omicron” that we heard so much of is now the latest surge / wave of SARS-CoV-2. Hospitals are again busy, but not all ICUs are, perhaps because BA.5 causes serious illness less frequently. So does that mean hospital management doesn’t need to entertain obtaining an eICU? Virtual ICUs are still extremely relevant: It’s not how much the hospitals can handle in their intensive care units or how full they are, but rather when a patient is in the ICU, do we want the patient to have the greatest probability of survival, the best clinical outcomes? If there is just one patient in the ICU, does that patient not deserve a US board certified critical care doctor to be the treating doctor, making critical decisions, as opposed to another doctor? The fact remains and is unchallenged that the intensivists improve patient outcomes in the critical care unit. And that’s basic, widely accepted modern medicine:
Surgeons do better surgery than non-surgeons, anesthesiologists administer better anesthesia than non-anesthesiologists, hematologists do better hematology than non hem-oncs, and critical care doctors do better intensive care unit treatment than non-intensivists, and so on throughout all physician specialties and sub-specialties. So BA.5 or not, TeleICU is needed.
June 26, 2022
The SCOTUS ruled effectively to cede control back to the individual states regarding the issue of abortion, by overturning an approximately 50 year old case, Roe v. Wade, which had made abortion a “right” at the federal level. States may outlaw abortion at the state level, or may not. Putting aside completely this contentious issue itself, it is worthwhile for administrators to consider what they personally believe to be a right when it comes to their hospitals’ critically ill patients. Do they have a right to be less likely to die? If that is a right, and they are less likely to die by conforming with the Leapfrog standard, having board certified critical care doctors involved in the patient care equation, to the extent that hospitals do not have boarded intensivists on staff, are they obligated to integrate TeleICU?
June 19, 2022
As adoption of virtual ICU as a means of providing patients often life-saving critical care became more widespread over the last 20 years, appropriate and relevant standards gained traction. ICU medicine as a medical specialty in the United States requires care provision by physicians who are board certified in the critical care specialty, in order meet the standard of care. Such physicians, variously called intensivists, critical care doctors, intensive care physicians, boarded intensivists, and so on, can provide care via telehealth according to The Leapfrog group. Leapfrog is the de facto standard with which hospital should comply. How do hospital system administrators view the relative importance of conformity with clinical standards in the context of high inflation and interest rate hikes from the fed? Nearly everything is more expensive these days, and the cost of capital is higher, and there is expected to be an economic slowdown. Should capital expenditure decisions made by hospitals for innovative technologies which enhance patient care be tied to national economics when people’s lives depend on it? Today’s blog entry asks more questions than it answers — these are simply difficult questions that must be grappled with.
June 13, 2022
With leaders like Jamie Dimon, CEO from JPMorgan Chase, saying there’s a economic hurricane looming and we just don’t know if it’s a smaller hurricane or more like a Hurricane Sandy, and Elon Musk indicating he will cut 10% of the Tesla workforce ahead of an expectation of an economic downturn, what does that mean for TeleICU decisions? Hospitals broadly are saying they are under financial pressure so while an argument can be made it’s not an optimal time for them to make capital expenditures, TeleICU need not cost signficant capital expenditure, can save expense, and can actually increase revenue. Time will tell if hospital administrators will use pure financial logic while doing the best for the patient to make their eICU go / no go decisions.
May 23, 2022
Up >50% in the last 2 weeks. Hospital admissions also up significantly though not as much as new cases. But for admitted patients, will eICU play a signficant role? All signs point to yes, particularly for those hospitals adapting the technology, but even for those that do not, they will undoubtedly transfer out critically ill patients to those that do have access to remote intensivist physicians.
March 20, 2022
New cases on the rise again in a leading country for Covid vaccine roll-outs. Keeping a watchful eye on it.
March 18, 2022
What is the state of telemedicine in Ukraine? Send your insights to us.
March 7, 2022
New Covid cases are on the decline. Will the trend continue?
February 24, 2022
Sonofi and GSK collaboration says their Covid vax protects as much as 100% against hospitalization. Is it a game changer?
January 30, 2022
Biden administration quietly decides to focus on hospitalizations and deaths due to Covid-19 (mortality) rather than daily new case count. An effective way to reduce deaths is to provide ICU patients the standard of care, which is management by a board certified critical care doctor via telehealth when there is otherwise no board certified intensivist available for bedside care.
September 13, 2021
Today, rules and regulations are in place in most industries in an effort to ensure that best practices and safety standards are followed.
May 1, 2021
Over the last decade, there has been significant growth in TeleICU.
April 3, 2021
Tele-hospitalists can contribute by filling gaps, taking over burdensome administrative tasks, and improving patient outcomes and patients’ experiences.
February 24, 2021
What role did tele-ICU play in meeting the challenges of the COVID-19 pandemic?
Physician Opportunities